Symptoms & Stages
The cause for the disruption of blood flow to the femoral head is unknown. Perthes disease does not have a strong genetic inheritance, and in fact, only about 5 percent of the patients have a family member with the condition. It also does not appear to be caused by direct hip injury.
Some studies have shown an association between Perthes disease and following factors: exposure to cigarette smoking, rare blood clotting disorders, hyperactivity and attention deficit disorder, and minor congenital abnormalities like inguinal hernias and undescended testes.
Perthes disease affects a wide age range of children (ages of 2 to 15) but the most common age range is between 4 and 9. Boys are four times more likely affected than girls. Ten percent of patients will have Perthes in both hips (referred to as bilateral Perthes disease). Usually one side is affected first and then the other side will get the disease a few years later. There is some variation in the frequency of Perthes disease between different regions and ethnic groups.
Symptoms of perthes:
In general, Perthes disease produces symptoms that have a gradual onset. Pain and limping are two common symptoms. The limping is often worse with activity or at the end of the day and often usually improves with rest. Pain is usually not specific to the hip. More often, children experience thigh or knee pain which delays proper diagnosis. Parents may notice that the movement of the affected hip is less than the unaffected side.
The diagnosis of Perthes disease requires careful history taking, physical examination, and x-rays. Since these symptoms and signs are not specific to the disease, x-rays are required to confirm Perthes. Since Perthes is a diagnosis of exclusion other childhood hip conditions that can mimic Perthes disease must be excluded such as the transient synovitis, corticosteroid induced osteonecrosis, sickle cell disease, and multiple epiphyseal dysplasia.
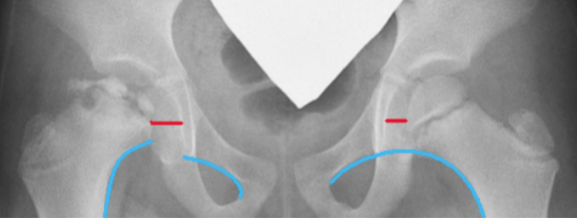
X-rays will show changes to the appearance and the shape of the femoral head. Based on the changes, the stage of the disease can be determined. Magnetic resonance imaging (MRI) using gadolinium can assess the blood flow to the femoral head and provide more detailed information about how much of the femoral head is affected.
Perthes disease goes through 4 stages numbered 1 to 4. These are called Waldenström radiographic stages as it was first described by Dr. Waldenström using x-rays. The duration of each stage is different with the stage 3 being the longest. Younger patients (those less than 6 years old when the disease began) tend to move through the stages faster and have better outcomes. Note that older patients (those over age 11) may not go through the stages as described below.
Stages of perthes:
1
STAGE 1: Initial or avascular necrosis stage
On x-rays, the femoral head looks whiter and smaller than the unaffected side due to the disruption of blood flow that causes bone death. Early flattening of the top of the femoral head or fracture line (called subchondral fracture or crescent sign) can be seen. This stage generally is less than one year.
2
STAGE 2: Fragmentation or resorptive stage
In this stage, the femoral head looks irregular and broken up (fragmented) with a more flattened appearance. These x-ray irregularities are due to the dead bone being removed by the healing process creating areas without bone (seen as dark areas on x-rays). The removal of the dead bone is called resorption and thus this stage is sometimes referred to as the resorptive stage. The femoral head can also appear to be moving out of the socket (called lateral subluxation or extrusion). This stage generally lasts 1 to 1 1/2 years.
3
STAGE 3: Reossification stage
In this stage, new bone (seen as increased white appearance of the femoral head) starts to fill in the areas where the dead bone has been removed. The newly-formed bone can be seen along the outer perimeter of the femoral head that gradually fills in towards the central area. Because the new bone is filling in, this stage is called the ossification stage. This stage is usually the longest stage and can take 2-3 years.
4
STAGE 4: Healed stage
In this stage, the appearance of the bone in the femoral head looks similar to the normal side. It is homogeneous and the irregular, fragmented appearance is no longer seen. The affected femoral head, however, can be enlarged (called coxa magna), flattened (coxa plana), and have a short, broad neck (coxa breva). The final shape of the femoral head at this stage (the degree of flattening or deformity) and how it fits the socket largely determines the long-term outcome. This is the stage where Stulberg radiographic classification is applied.
Within five years, most of the patients will be able to return to full activities including sports with minimal symptoms once the femoral head has healed. Even with that said, the childhood journey of Perthes can be quite frustrating to parents (captured in the above image) when trying to explain the complexity of the disease to others.
The long-term prognosis (20-40 years later) depends on the shape of the femoral head and how well it fits the socket at the time of skeletal maturity (approximately age 14 for girls and age 16 for boys). If the femoral head is very flat or irregular and does not fit the socket well, there is a high chance of getting degenerative arthritis and need for a hip replacement as an adult, even as early as the thirties and forties. Children who are older at the onset of Perthes and those who have the femoral head move out of the socket are more likely to require a hip replacement.
Shape of the femoral head, age at onset of disease, and the amount of disease involvement affect outcome defined as developing degenerative arthritis of the hip joint. Younger children (under 6 years old at the onset of the disease) tend to have a better outcome with less lasting deformity of the femoral head and a shorter duration of disease. Patients over 8 years tend to have a worse outcome.
For patients with Perthes who ultimately require a hip replacement as an adult, the outcomes are quite good. In one report, over 95% of hip replacements were doing well at 15 years after surgery, with a marked improvement in function. Unfortunately, the complication rate of surgery was higher than the typical hip replacement, particularly with regard to sciatic nerve injuries. In another study, patients with Perthes and an abnormal socket had a more than two and a half times the risk of postoperative hip dislocation in the first six months after surgery. Long-term outcomes in this study however, revealed that patients with Perthes did as well as others having a hip replacement.
Donate To Perthes Research
For more information about Legg-Calve-Perthes disease and current studies, please visit the International Perthes Study Group (IPSG). They are working hard to find the exact cause, and better yet, a cure for Perthes disease. Please consider making a donation to the IPSG to help fund their efforts and further support this important research.